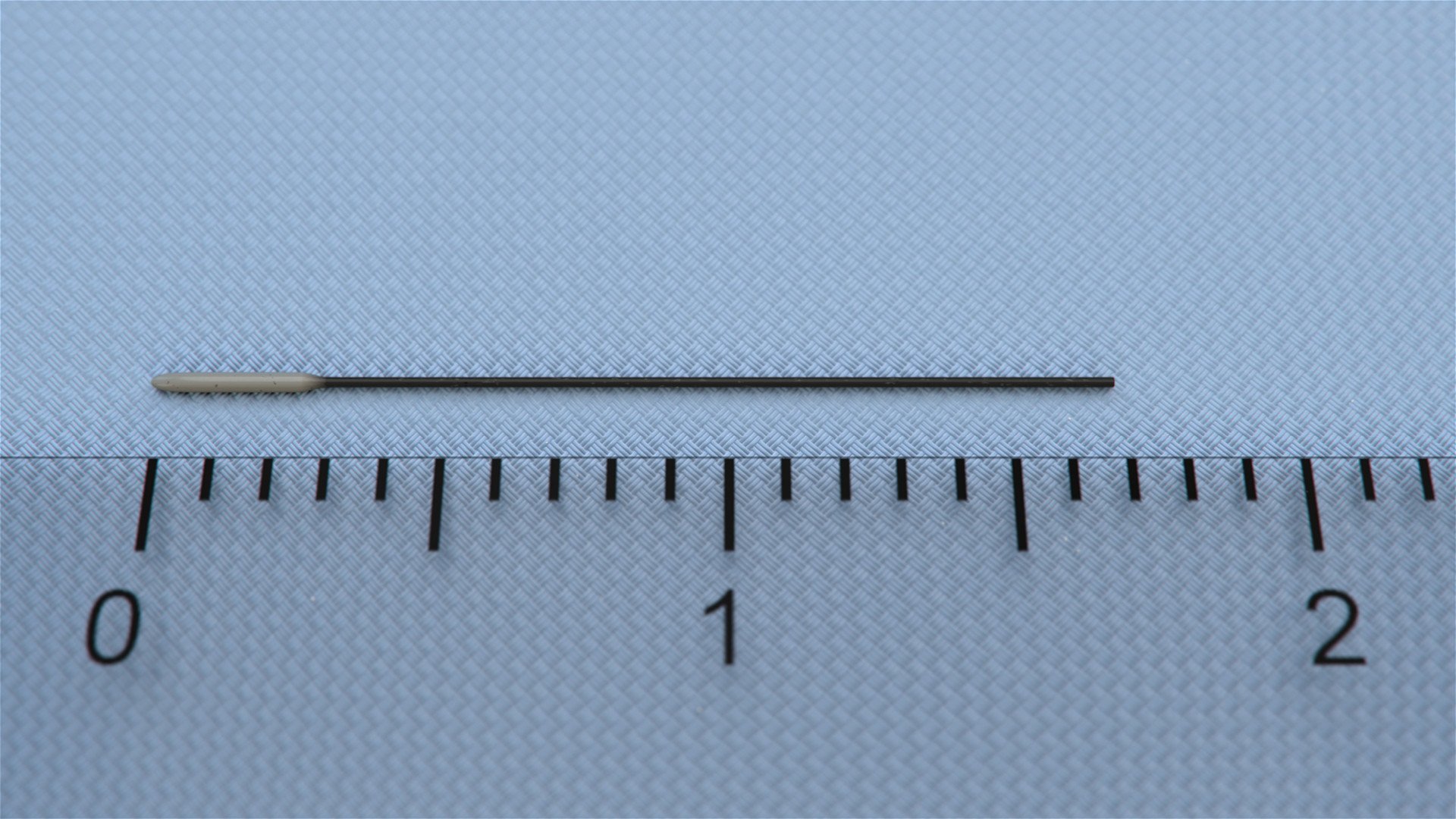
Silicone Coated MCAO Monofilament Suture
$300.00 – $350.00
The MCAO Monofilament Sutures are made of silicone-wrapped nylon thread, to ensure that the suture occlusion can easily enter the common carotid artery from the external carotid artery, and finally enter the MCA branch of the internal carotid artery without piercing the inner wall of the vessel and changing the original direction of the vessel. It can also ensure a higher success rate of modeling meanwhile achieving a more realistic modeling effect.
ConductScience offers the Silicone Coated MCAO Monofilament Suture.
Description
Specifications
*All Mouse Models – Total Lenght= 30mm. Coating Lenght 3~4.
*All Rat Models – Total Lenght= 50mm. Coating Lenght=5~6
Features
Shape/Material
- Monofilament material
- Silicone-coated
- Smooth passage through tissues
- Biocompatible
Size Options
- Various sizes
- Different experimental needs
- Uniform diameter
- Uniform consistency
Visibility
- Enhanced visibility for
- certain imaging techniques
- Uniform diameter
Research
- Tailored
- For neurological research
- Stroke studies
- Made of silicone, ideal to improve the reuse probability of suture occlusion
- The use of nylon thread with better flexibility allows for a higher success rate of modeling
- The unique technique of open-molded manufacturing provides uniform height and further ensures a stable MCAO model
- A cylinder-like silicone head ensures that the blood flow decreases immediately after the suture occlusion enters the MCA
Introduction
Middle Cerebral Artery Occlusion (MCAO) is a commonly used focal ischemia model in rodents for stroke research. The endovascular suture or filament technique is popular in vivo model of MCAO that allows reproducible middle cerebral artery (MCA) infractions, does not require craniectomy, and allows reperfusion by the withdrawal of the occluding filament. First described by Koizumi et al. in 1986 and improved upon by Longa et al. in 1989, the method achieves the cessation of blood flow and subsequent brain infarction by forwarding a surgical filament via the internal carotid artery until the tip occludes the origin of MCA. However, the endovascular filament MCAO fails to mimic clinical situations.
On the other hand, the embolic MCAO first described by Kudo et al. is another popular model that closely mimics human ischemic stroke. Thromboembolic clot models and non-thromboembolic (microsphere or macro-sphere induced) stroke models are the two major types of embolic MCAO. Thromboembolic MCAO is achieved by injection of in vitro clots or via in situ clotting by the endovascular installation of thrombin. This model of MCAO closely reflects the pathophysiology of human cardioembolic stroke. The composition of the clot (thromboembolic model) and the size of the spheres (non-thromboembolic model) were used to have a direct effect on the quality of the MCAO and the infraction induced.
Protocol
Perform the MCAO in a sterile environment. Before beginning with the surgical processes all tools and equipment including the surgery area must be sterilized and sanitized.
Pre-surgery procedures
Weigh the subject before beginning the procedures. Using isoflurane (4-5% for induction, 2-3% for maintenance) in 30% O2 and 70% N2O, anesthetize the subject. Ensure the subject is sufficiently anesthetized by pinching both the rear feet and observing for any movements. Apply a lubricant ophthalmic ointment to both eyes to prevent eye desiccation during the procedures. Shave the fur off the head and neck region and place the subject in a supine position on a heated pad with all its paws tapped to the surface. Insert a rectal probe to maintain constant core temperatures of 36.5-37.5 °C. Tape down the tail of the subject to the probe.
It is important to note that occlusion-inducing materials and methods may slightly vary depending on species, strains, and weights.
Endovascular filament MCAO
- Make a midline neck incision between the manubrium and jaw under a dissecting microscope.
- Bluntly divide the underlying submandibular gland, leaving the left gland in situ, and retract the right gland cranially and secure it along with the sternocleidomastoid muscle.
- Carefully divide the exposed division of the omohyoid muscle covering the carotid sheath.
- Separate and isolate the right common carotid artery (CCA) from the vagus nerve and its sheath.
- Dissect the external carotid artery (ECA) near its bifurcation into lingual and maxillary arteries, cauterize and divide it with micro-scissors.
- Prepare two loose collar sutures (7-0 silk) around the proximal internal carotid artery (ICA) just above the CCA bifurcation.
- Temporarily close the CCA using a vessel clip and verify cortical perfusion values.
- Next, using a vessel clip above the two loose collar sutures, temporarily close ICA to avoid retrograde flow during arteriotomy.
- Perform arteriotomy in the reflected ECA close to the stump.
- Introduce the heat blunted silicone coated 7-0 nylon suture via the arteriotomy in the ECA and advance till vessel clip in ICA. Gently tighten the two-loose collar suture around the proximal ICA to avoid reflux blood flow, without traumatizing the arterial wall and then withdrawing the vessel clip.
- Advance the occluding suture via the internal carotid artery (ICA) towards the cranial base until a mild resistance is observed. Tighten the two collar sutures around the filament.
- For the transient model of MCAO, gently withdraw the filament after the pre-defined duration. Cauterize the base of ECA and loosen the collar sutures at the proximal ICA to restore carotid flow.
- Lay the submandibular gland and sternocleidomastoid over the operative field and close the incision using a tissue adhesive or an absorbable suture or a metal staple.
Embolic MCAO
- Under a dissecting microscope make a 2 cm midline incision. While exposing the surgical field using retractors, dissect the right CCA, ECA, ICA, and pterygopalatine artery (PPA) away from the surrounding nerves and fascia.
- Place a 5-0 silk suture under the CCA. Tie it into a slip knot and pull taut towards the body.
- Dissect the ECA and its two branches, the occipital artery (OA) and the superior thyroid artery (STA). Using a veterinary electrosurgical unit, coagulate the two branches.
- Place two 6-0 silk sutures under the ECA, one towards the head and the other towards the body. Tie the suture towards the head tightly and loosely knot the other suture.
- Tie the PPA with a 6-0 suture. Using a slip knot with 6-0 suture or microvascular clip, tie/clip the ICA.
- Between the two sutures of the ECA, cut a small incision in the ECA and insert the modified PE-%) the tube containing the blood clot. Advance the tubing to the bifurcation of the CCA. Tighten the loose suture of the ECA around the lumen, such that to allow mobility of the tube.
- Free the stump by cutting off the ECA at the incision site. Position the stump below the bifurcation of ECA and the ICA. Open the ICA and advance the tube into it until the tip of the catheter reaches the origin of MCA.
- Inject the clot through the modified PE-50 catheter along with 10 μl of saline over 10 seconds using a 100 μl Hamilton syringe.
- Withdraw the catheter from the ECA 5 min later. Tie the ECA and reopen CCA. Suture the incision on the neck.
Apparatus and Equipment
Evaluation of intraarterial administration of norcantharidin
Khan et al. used spontaneously hypersensitive rats and divided them into 3 treatment groups: treated (90-minute MCAO followed by intraarterial drug administration), controls (MCAO followed by intraarterial vehicle administration), and shams (surgery but no MCAO). The occlusion of the MCA was performed using the endovascular filament technique. Subjects that showed left-side weakness on the upright test underwent removal of the suture after 90 minutes of stroke time. A PE-20 tube was routed into the proximal ICA using the ECA stump through which the treated group received NCTD (0.5 mg/kg) while control received only normal saline and dimethyl sulfoxide (DMSO) (1:5), infused at a rate of 0.10 ml/min for 5 to 7 minutes. Subjects’ sensorimotor function was tested on the ladder rung test. It was observed that the treated group had significantly higher scores on the Garcia neurological test and in the ladder rung test showed significantly higher average forelimb fault scores and stability than the controls. The investigators concluded that endovascular administration of neuroprotective agents has the potential efficacy in shielding the subjects from neurotoxic consequences of ischemia and reperfusion.
Investigation of the effect of OTULIN on ischemic stroke model
Xu et al. investigated in vitro and in vivo anti-inflammatory effects of OTULIN in ischemic stroke models by overexpression of the OTULIN gene. Sprague-Dawley rats received an intracerebroventricular (ICV) injection of overexpressing OTULIN (LV-OTULIN) or control lentivirus (LV-Scramble). After seven days post-injection, the rats either underwent transient MCAO (tMCAO) or were treated intraperitoneally with lipopolysaccharide (LPS) injections (500 μg/kg) diluted with sterile PBS. The results from the assessments performed in the investigation suggested the potential therapeutic target provided by OTULIN by amelioration of excessive microglial cells and neuroinflammation activation via repressing the NF-κB signaling pathway for ischemic stroke.
Evaluation of rapamycin in preventing cerebral stroke
Wu et al. investigated the potential benefit of activation or inhibition of the mTOR pathway in the ischemic stroke model. The subjects were divided into two groups: rapamycin pre-treatment group and rapamycin post-treatment group. The pre-treatment group received 3 mg/kg rapamycin injected intraperitoneally once a day for 3 consecutive days. After 24 hours of the last injection, the subjects underwent MCAO. Post-treatment group received the same dosage of rapamycin 6 hours after MCAO for another 3 consecutive days. Both rapamycin treated groups had a marked decrease in infarct volume in comparison to the vehicle-only treated group. Further, reduction in neural apoptosis and increase activation of autophagy was also observed in the rapamycin treated groups.
Strenght and limitations
The endovascular filament MCAO has been a popular model in mechanism-driven stroke research. However, embolic MCAO has seen a growing interest. As opposed to the intraluminal suture technique, the embolic model closely mimics the human ischemic stroke, thus, making it a more suitable model for preclinical investigation of thrombolytic therapy.
In comparison to other models of MCAO, the filament technique is relatively non-invasive. The method avoids craniotomy which tends to influence the blood-brain barrier permeability and intracranial pressure. The technique has seen popularity in studies of cellular injury and neuroprotection. The method can create consistent infractions and has a high-throughput potential. The use of monofilaments enables achieving permanent or transient occlusions in the subject. However, reperfusion achieved by this method is ad hoc in nature as opposed to that occurring in the human ischemic stroke. Other downsides to the method include subarachnoid hemorrhage, tracheal edema, and paralysis of muscles of mastication and swallowing due to the injury of the ECA. Despite these factors, the method has relevant use in endovascular therapy of ischemic stroke due to large vessel occlusion.
The embolic MCAO provides two techniques to occlude the MCA. The first method uses the introduction of a clot obtained from spontaneously formed or thrombin-induced thrombotic material (from autologous or heterologous blood). This model closely imitates the clinical situations in comparison to other methods. Therefore, it serves as an ideal model for the analysis of spontaneous or iatrogenic lysis by recombinant tissue plasminogen activator (rt-PA) in experimental thrombolysis. However, the nature of the clot varies from that of humans. Further, the quality of the MCAO is highly variable and dependent on the number and size of the clots and the route of application. This method also requires the use of larger experimental cohorts to obtain statistically significant results. To overcome this disadvantage, the MCAO can be induced using non-thromboembolic micro or macrospheres. Though, this method is a departure from the imitation of the clinical situation as seen with the thromboembolic method. Microspheres enable microembolization of multiple vessels resulting in multifocal and heterogeneous infarcts that develop up to 24 hours after injection. On the other hand, macro-spheres allow postponing of the occlusion to enable ischemia induction while the subject lies in an MRI or PET scanner.
Summary
- Endovascular filament and embolic MCAO are two popular focal ischemic stroke models.
- Endovascular filament MCAO does not require craniotomy and allows for both permanent and transient occlusions of the MCA.
- Endovascular filament MCAO does not closely mimic clinical situations. However, it is a relevant model in endovascular therapy.
- Embolic MCAO has two prominent categories based on the occluding material; thromboembolic clot and non-thromboembolic models.
- Embolic MCAO closely mimics the human ischemic stroke. However, there is high variability of the MCAO.
- The thromboembolic clot can be sourced from spontaneously formed or thrombin-induced thrombotic material.
- Microspheres enable microembolization of multiple vessels.
- Macrospheres allow delaying of occlusion to induce a stroke.
References
- Chiang T, Messing RO, Chou W-H. Mouse model of middle cerebral artery occlusion. J Vis Exp. 2011;955(48):9-10. doi:10.3791/2761.
- Shimamura N, Matchett G, Tsubokawa T, Ohkuma H, Zhang J. Comparison of silicon-coated nylon suture to plain nylon suture in the rat middle cerebral artery occlusion model. J Neurosci Methods. 2006;156(1-2):161-165. doi:10.1016/j.jneumeth.2006.02.017.
- Chen Y, Ito A, Takai K, Saito N. Blocking pterygopalatine arterial blood flow decreases infarct volume variability in a mouse model of intraluminal suture middle cerebral artery occlusion. J Neurosci Methods. 2008;174(1):18-24. doi:10.1016/j.jneumeth.2008.06.021.
- Lee S, Hong Y, Park S, Lee S-R, Chang K-T, Hong Y. Comparison of surgical methods of transient middle cerebral artery occlusion between rats and mice. J Vet Med Sci. 2014;76(12):1555-1561. doi:10.1292/jvms.14-0258.
Additional information
| Package Size | 50pcs |
|---|---|
| Species | Mouse, Rat |
| Size | >35gr, >400gr, <200gr, 15-20gr, 21-25gr, 26-30gr, 31-35gr, 200-250gr, 251-280gr, 281-330gr, 331-400gr |
You must be logged in to post a review.
Related products
-

Drosophila Bottles,PP, Round Bottom
$175.50 – $238.00 Select options This product has multiple variants. The options may be chosen on the product page -

Breathing Circuit
$30.00 – $95.00 Select options This product has multiple variants. The options may be chosen on the product page -
Sale!

Elschling 1×2 Teeth Tissue Forceps
$730.00Original price was: $730.00.$700.00Current price is: $700.00. Add to cart -
Stille Dressing Forceps w/Flat Tips
Read more



Reviews
There are no reviews yet.